Anatomy of female pelvic organs: Pelvic part of the female uterus measures 13 cm with a diameter of 5 mm. It lies close to the supravaginal part of the cervix (1.5 cm).
It is comparatively constricted
- where it crosses the brim,
- where crossed by uterine artery and,
- in the intravesical part.
The uterus is likely to be damaged during hysterectomy at the infundibulopelvic ligament, by side of the cervix, at the vaginal angle, and during posterior peritonization.
Pelvic cellular tissues (endopelvic fascia), ligaments, perineal body, pelvic floor muscles (levator ani), support the pelvic organ and counteract the downward thrust of increased intra-abdominal pressure. This prevents pelvic organ prolapse.
 |
| Female Pelvic |
What is involved in the Anatomy of Female pelvic organs?
These All organs are well short defined in the posts. This is basically an Outline of the post for a better understanding. - Explore the Anatomy of female Pelvic organs.
Female pelvic organs include:
◼ External Genitalia (SYN: Vulva, Pudendum)
◾ Mons Veneris (mons pubis)
◾ Labia Majora
◾ Labia Minora
◾ Clitoris
◾ Vestibule (there are four openings into the vestibule)
▪ Urethral Opening
▪ Vaginal Orifice and Hymen
◾ Bartholin's Gland
▪ Vestibular Bulbs
◾ Perineum
▪ Blood Supply of the vulva
▪ Nerve Supply of the vulva
◼ Internal Genital Organs
◾ Vagina
▪ Walls
▪ Fornices
▪ Relations
. Anterior
. Posterior
. Lateral Walls
▪ Structures
▪ Epithelium
▪ Secretion
▪ Blood Supply
▪ Nerve Supply
Female pelvic organ External Genitalia
The vulva includes mons veneris, labia majora, labia minora, clitoris, vestibule, and conventionally the perineum. These are all visible on external examination. It is, therefore, bounded anteriorly by the mons veneris, laterally by the labia major, and posteriorly by the perineum.
Mons Veneris - mons pubis
It is the pad of subcutaneous adipose connective tissue lying in front of the pubis and, in the adult female, is covered by hair.
Labia Majora
In the female pelvic organ, The vulva is bounded on each side by the elevation of the skin and subcutaneous tissue, which form the labia majora. They are continuous where they join medially to form the posterior commissure in front of the anus. The inner surface of the labia majora is hairless. The labia majora are covered with squamous epithelium and contain sebaceous glands, sweat glands, and hair follicles.
Beneath the skin, there are dense connective tissue and adipose tissue. The adipose tissue is richly supplied by the venous plexus, which may produce hematoma if injured during childbirth. The labia majora are homologous with the scrotum in the male. The round ligaments terminate at its anterior third.
Labia Minora
Labia minora are two thick folds of skin, devoid of fat, on either side just within the labia majora. Except in the parous women, they are only exposed when the labia majora are separated. Anteriorly, they are divided to enclose the clitoris and unite with each other in front and behind the clitoris to form. the prepuce and frenulum, respectively. The lower. The portion of the labia minora fuses across the midline to form a fold of skin known as a fourchette.
It is s usually injured during childbirth. Between the fourchette and the vaginal orifice is the fossa navicularis. The labia minora do not contain hair follicles. The folds contain connective tissues, numerous sebaceous glands, erectile muscle fibers, and numerous vessels and nerve endings. It is homologous to the ventral aspect of the penis.
Clitoris
The clitoris is a small cylindrical erectile body, measuring about 2.5 cm situated in the most anterior part of the vulva. It consists of glans, a body, and two crura. The glans are covered by squamous epithelium and are richly supplied with nerves.
The vessels of the clitoris are connected with the vestibular bulb and are liable to be injured during childbirth. The clitoris is an analogue to the penis in the male, but it differs basically in being entirely separate from the urethra. It is attached to the undersurface of the symphysis pubis by the suspensory ligament.
Vestibule
The vestibule is a triangular space bounded anteriorly by the clitoris, posteriorly by the fourchette, and on either side by labium minus. There are four openings into the vestibule.
Urethral opening of the female pelvic
The opening is situated in the midline, just in front of the vaginal orifice about 1-1.5 cm below the pubic arch. The paraurethral ducts open either on the posterior wall of the urethral orifice or directly into the vestibule.
 |
| The vaginal vulva |
Vaginal orifice and hymen Female pelvic
The vaginal orifice lies in the posterior end of the vestibule and is of varying size and shape. In virgins and nulliparae, the opening is closed by the labia minora but in parous, it may be exposed. It is incompletely closed by a septum of the mucous membrane, called the hymen.
The membrane varies in shape but is usually circular or crescentic in virgins.
The hymen is usually ruptured at the consummation of marriage. During childbirth, the hymen is extremely lacerated and is later represented by cicatrized nodules of varying sizes, called the carunculae myrtiformes. On both sides, it is lined by stratified squamous epithelium.
Bartholin's Gland
The Bartholin's glands are situated in the superficial perineal pouch, close to the posterior end of the vestibular bulb. They are pea-sized, of about 0.5 cm, and yellowish-white in color.
 |
| Exposition of a superficial perineal pouch with vestibular bulb and Bartholin's gland |
During sexual excitement, it secretes abundant alkaline mucus which helps in lubrication, Contraction of bulbocavernosus helps squeeze the secretion. The glands are compound racemose variety and are lined by columnar epithelium.
Each gland has got a duct that measures about 2 cm and opens into the vestibule, outside the hymen at the junction of the anterior two-thirds and posterior one-third in the groove between the hymen and the labium minus. The duct is lined by columnar epithelium but near its opening by stratified squamous epithelium. The Bartholin's gland corresponds to the bulbourethral gland of males.
Vestibular Bulbs
These are bilateral elongated masses of erectile tissues situated beneath the mucous membrane of the vestibule. Each bulb lies on either side of the vaginal orifice in front of the Bartholin's gland and is incorporated within the bulbocavernosus muscles. They are homologous to the single bulb of the penis and corpus spongiosum in the male. They are likely to be injured during childbirth with brisk hemorrhage.
Perineum
The details of the anatomy of the perineum are described later in the post (Obstetrical Perineum-body, central point).
Blood supply of the vulva
Arteries of the vulva
- Branches of an internal pudendal artery- the chief being labial, transverse perineal, artery to the vestibular bulb, and deep and dorsal arteries to the clitoris.
- Branches of the femoral artery- superficial and deep pudendal.
Veins of the Vulva
The veins from plexuses and drain into:
- Internal pudendal vein
- Vesical or vaginal venous plexus
- Long saphenous vein.
Varicosities during pregnancy are not uncommon and may rupture spontaneously causing visible bleeding or hematoma formation.
Nerve supply of the vulva
The supply is through bilateral spinal somatic nerves. The anterosuperior part is supplied by the cutaneous branches from the genitofemoral nerve (L1 and L2) and the posteroinferior part by the pudendal branches from the posterior cutaneous nerve of the thigh (S2,3,4). Between these groups, the vulva is supplied by the labial and perineal branches of the pudendal nerve (S2,3,4).
Internal Genital Female pelvic organs
The internal genital organs in females include the vagina, uterus, fallopian tubes, and ovaries. These organs are placed internally and require special instruments for inspection.
 |
| Fig. 1.3: Mid-sagittal section of the female pelvis showing the relative position of the pelvic organs |
Vagina
The vagina is a fibromusculomembranous sheath communicating the uterine cavity with the exterior at the vulva. It constitutes the excretory channel for uterine secretion and menstrual blood. It is the organ of copulation and forms the birth canal of parturition. The canal is directed upwards and backward forming an angle of 45° with the horizontal in an erect posture.
The long axis of the vagina almost lies parallel to the plane of the pelvic inlet and at right angles to that of the uterus. The diameter of the canal is about 2.5 cm, being widest in the upper part and narrowest at its introitus. It has got enough power of distensibility as evident during childbirth.
Walls of vagina
Vagina has got an anterior, a posterior, and two lateral walls. The anterior and posterior walls are apposed together but the lateral walls are comparatively stiffer especially at its middle, as such it looks 'H' shaped on a transverse section. The length of the anterior wall is about 7 cm and that of the posterior wall is about 9 cm. The upper end of the vaginal is above the pelvic floor.
Vagina Fornices
The fornices are the clefts formed at the top of the vagina (vault) due to the projection of the uterine cervix through the anterior vaginal wall, where it is blended inseparably with its wall. There are four fornices one anterior, one posterior, and two lateral; the posterior one being deeper and the anterior, most shallow one.
Relations of vagina
Anterior
The upper one-third is related to the base of the bladder and the lower two-thirds are with the urethra, the lower half of which is firmly embedded with its wall.
Posterior
The upper one-third is related to the pouch of Douglas, the middle-third with the anterior rectal wall separated by the rectovaginal septum, and the lower-third is separated from the anal canal by the perineal body (Fig. 1.3).
Lateral walls
The upper one-third is related to the pelvic cellular tissue at the base of a broad ligament in which the ureter and the uterine artery lie approximately 2 cm from the lateral fornices. The middle-third is blended with the levator ani and the lower-third is related with the bulbocavernosus muscles, vestibular bulbs, and Bartholin's glands.
Structures of vagina
Layers from within outwards are
(1) mucous coat which is lined by stratified squamous epithelium without any secreting glands;
(2) submucous layer of loose areolar vascular tissues;
(3) muscular layer consisting of indistinct inner circular and outer longitudinal and;
(4) fibrous coat derived from the endopelvic fascia which is tough and highly vascular.
Epithelium in vagina
The vaginal epithelium is under the action of sex hormones. At birth and up to 10-14 days, the epithelium is stratified squamous under the influence of maternal estrogen circulating in the newborn. Thereafter, up to prepuberty and in postmenopause, the epithelium becomes thin, consisting of few layers only.
From puberty till menopause, the vaginal epithelium is stratified squamous and devoid of any gland. Three distinct layers are defined-basal cells, intermediate cells, and superficial cornified cells. The intermediate and superficial cells contain glycogen under the influence of estrogen. These cells become continuous with those covering the vaginal portion of the cervix and extend up to the squamocolumnar junction at the external os.
The superficial cells exfoliate constantly and more so in inflammatory or neoplastic conditions. Replacement of the superficial cells occurs from the basal cells. When the epithelium is exposed to the dry external atmosphere, keratinization occurs. Unlike skin, it does not contain hair follicles, sweat, and sebaceous glands.
Vaginal Secretion
The vaginal secretion is very small in an amount sufficient to make the surface moist. Normally, it may be little excess in mid-menstrual or just prior to menstruation, during pregnancy, and during sexual excitement. The secretion is mainly derived from the glands of the cervix, uterus, transudation of the vaginal epithelium, and Bartholin's glands (during sexual excitement).
The pH is acidic and varies during different phases of life and the menstrual cycle. Conversion of glycogen in the exfoliated squamous cells to lactic acid by the Doderlein's bacilli is dependent on estrogen. As such, the pH is more acidic during the childbearing period and ranges between 4 and 5.5 with an average of 4.5. The pH is highest in the upper vagina because of contaminated cervical secretion (alkaline).
The vaginal secretion consists of tissue fluid, epithelial debris, some leukocytes (never contains more than an occasional pus cell), electrolytes, proteins, and lactic acid (in a concentration of 0.75%). Apart from Doderlein's bacilli, it contains many pathogenic organisms including Cl. welchii. The glycogen content is highest in the vaginal fornix to the extent of 2.5-3 mg% and is lowest in the lower third being 0.6-0.9 mg%.
Doderlein's bacillus: It is a rod-shaped gram-positive bacillus that grows anaerobically on acid media. It appears in the vagina 3-4 days after birth and disappears after 10-14 days. It appears again at puberty and disappears after menopause. It probably comes from the intestine. Its presence is dependent on estrogen, and its function is to convert the glycogen present in the vaginal mucosa into lactic acid so that the vaginal pH is. maintained towards the acidic side. This acid pH prevents the growth of other pathogenic organisms.
Blood Supply in the vagina
The arteries involved are
(1) cervicovaginal branch of the uterine artery,
(2) vaginal artery-a branch of the anterior division of the internal iliac or in common origin with the uterine,
(3) middle rectal, and
(4) internal pudendal. These anastomose with one another and form two azygos arteries anterior and posterior.
Veins drain into internal iliac and internal pudendal veins.
Nerve Supply in the vagina
The vagina is supplied by sympathetic and parasympathetic from the pelvic plexus. The lower part is supplied by the pudendal nerve.
The uterus position Measurements and parts
The uterus is a hollow pyriform muscular organ situated in the pelvis between the bladder in front and the rectum behind.
Position
Its normal position is one of the anteversion and anteflexion. The uterus usually inclines to the right (dextrorotation) so that the cervix is directed to the left (levorotation) and comes in close relation. with the left ureter.
Measurements and parts
The uterus measures about 8 cm long, 5 cm wide at the fundus, and its walls are about 1.25 cm thick. Its weight varies from 50-80 g. It has got the following parts.
Uterus Corpus, Isthmus, and Cervix
Body or corpus
The body is further divided into the fundus the part which lies above the openings of the uterine tubes. The body properly is triangular and lies between the openings of the tubes and the isthmus. The superolateral angles of the body of the uterus project outwards from the junction of the fundus and body and are called the cornua of the uterus. The uterine tube, round ligament, and ligament of the ovary are attached to each cornu.
Isthmus
The isthmus is a constricted part measuring about 0.5 cm situated between the body and the cervix. It is limited above by the anatomical internal os and below by the histological internal os (Aschoff). Some consider the isthmus as a part of the lower portion of the body of the uterus.
Cervix
The cervix is the lowermost part of the uterus. It extends from the histological internal os and ends at the external os which opens into the vagina after perforating the anterior vaginal wall. It is almost cylindrical in shape and measures about 2.5 cm in length and diameter. It is Divided Into a supravaginal part- the part lying above the vagina and a vaginal part which lies within the vagina, each measuring 1.25 cm. In nulliparous, the vaginal part of the cervix is conical with the external os looking circular, whereas in parous, it is cylindrical with the external os having bilateral slits. The slit is due to invariable. tear of the circular muscles surrounding the external os and gives rise to anterior and posterior lips of the cervix.
Uterus Cavity female pelvic organs anatomy
The cavity of the uterine body is triangular on a coronal section with the base above and the apex. below. It measures about 3.5 cm. There is no cavity in the fundus. The cervical canal is fusiform and measures about 2.5 cm. Thus, the normal length of the uterine cavity including the cervical canal is usually 6-7 cm.
Uterus Relations
Anteriorly
Above the internal os, the body forms the posterior wall of the ureterovesical pouch. Below the internal os, it is separated from the base of the bladder by loose areolar tissue.
Posteriorly
It is covered by the peritoneum and forms the anterior wall of the pouch of Douglas containing coils of the intestine,
Laterally
The double folds of the peritoneum of the broad ligament are attached laterally between which the uterine artery ascends up. Attachment of the Mackenrodt's ligament extends from the internal os down to the supravaginal cervix and lateral vaginal wall. About 1.5 em away at the level of internal os a little nearer on the left side is the crossing of the uterine artery and the ureter. The uterine artery crosses from above and in front of the ureter, soon before the ureter enters the ureteric tunnel.
Uterus body structures anatomy
Body- The wall consists of 3 layers from the outside. inwards:
Perimetrium- It is the serous coat that invests the entire organ except on the lateral borders. The peritoneum is intimately adherent to the underlying muscles.
Myometrium- It consists of thick bundles of smooth muscle fibers held by connective tissues and is arranged in various directions. During pregnancy, however, three distinct layers can be identified-outer longitudinal, middle interlacing, and inner circular.
Endometrium- The mucous lining of the cavity is called the endometrium. As there is no submucous layer, the endometrium is directly opposed to the muscle coat. It consists of lamina propria and surface epithelium. The surface epithelium is a single layer of ciliated columnar epithelium. The lamina propria contains stromal cells, endometrial glands, vessels, and nerves. The glands are simple tubular and lined by mucus-secreting non-ciliated. columnar epithelium which penetrates the stroma and sometimes even enters the muscle coat. All the components are changed during menstrual cycles. The endometrium is changed to decidua during pregnancy.
From what mainly Cervix composed of
The Cervix is composed mainly of fibrous connective tissues. The smooth muscle fibers average 10-15%. Only the posterior surface has got a peritoneal coat.
Epithelial Lining of the cervix Endocervical canal and glands
There is a medium ride on both the anterior and posterior surface of the canal from which transverse folds radiate. This arrangement is called arborvitae uteri. The canal is lined by a single layer of tall columnar epithelium with basal nuclei. Those placed over the top of the folds are ciliated. There are patches of cubical basal or reverse cells underneath the columnar epithelium. These cells may undergo squamous metaplasia or may replace the superficial cells.
The glands which dip into the stroma are of a complex racemose type and are lined by secretory columnar epithelium. There is no stroma unlike the corpus and the lining epithelium rests on a thin basement membrane. The change in the epithelium and the glands during the menstrual cycle and pregnancy are not so much as those in the endometrium.
Portio vaginalis
It is covered by stratified squamous epithelium and extends right up to the external os where there is an abrupt change to columnar type.
The transitional zone (transformation zone). maybe of 1-10 mm width with variable histological features. The zone consists of endocervical stroma and glands covered by squamous epithelium. The zone is not static but changes with the hormone level of estrogen. The site is constantly irritated not only by hormones but also by infection and trauma. Thus, there is more chance of severe dysplasia, carcinoma in situ, or even invasive carcinoma in this zone.
Secretion endometrial secretion
The endometrial secretion is scanty and watery. The physical and chemical properties of the cervical secretion change with menstrual cycles and with pregnancy. The cervical glands secrete an alkaline mucus with pH 7.8. The mucus is rich in fructose, glycoprotein, and mucopolysaccharides. It also contains sodium chloride. Fructose has got a nutritive function for spermatozoa. Under estrogenic stimulation, the glycoprotein network is arranged parallel to each other thus facilitating sperm ascent. Progesterone produces interlacing bridges thereby preventing sperm penetration. Cervical mucus contributes significantly to normal vaginal discharge.
A part forms the mucus plug which functionally closes the cervical canal and has got bacteriolytic properties.
Uterus arterial blood supply
The arterial supply is from the uterine artery-one on each side. The artery arises directly from the anterior division of the internal iliac or in common with the superior vesical artery. The other sources are ovarian and vaginal arteries to which the uterine arteries anastomose.
The uterine artery crosses the ureter anteriorly about 1.5 cm away at the level of internal os before it ascends up along the lateral border of the uterus in between the leaves of the board ligament.
Veins: The venous channels correspond to the arterial course and drain into internal iliac veins.
Uterus Nerve supply
The nerve supply of the uterus is derived principally from the sympathetic system and partly from the parasympathetic system. Sympathetic components are from T5 and T6 (motor) and T10 to L1 spinal segments (sensory). The somatic distribution of uterine pain is that area of the abdomen supplied by T10 to L1. The parasympathetic system is represented on either side by the pelvic nerve which consists of both motor and sensory fibers from S2, S3, S4, and ends I in the ganglia of Frankenhauser which lies on either side of the cervix.
The cervix is insensitive to touch, heat, and also. when it is grasped by any instrument. The uterus, too. is insensitive to handling and even to incision over its wall.
Changes of Uterus with Age
At birth, the uterus lies in the false pelvis; the cervix is much longer than the body. In childhood, the proportion is maintained but reduced to 2:1. At puberty, the body is growing faster under the action of ovarian steroids (estrogens) and the proportion is reversed to 1:2 and following childbirth, it becomes even 1:3. After menopause the uterus atrophies; the overall length is reduced; the walls become thinner, less muscular but more fibrous.
 |
| Changes in the size of the uterus from birth to 75 years of age. Note the change in the relation of the cervix to the body |
Position of the Uterus
The normal position of the uterus is anteversion and anteflexion. Anteversion relates the long axis of the cervix to the long axis of the vagina which is about Anteflexion relates the long axis of the body to the long axis of the cervix and is about 120°. In about 15-20%, normally the uterus remains in a retroverted position. In erect posture, the internal os lies on the upper border of the symphysis pubis and the external os lies at the level of ischial spines.
Fallopian tube Parts, Structures, Functions, and Blood supply
The uterine tubes are paired structures, measuring about 10 cm (4") and are situated in the medial three fourth of the upper free margin of the broad ligaments. Each tube has got two openings, one communicating with the lateral angle of the uterine cavity, called a uterine opening, and measures I mm in diameter, the other is on the lateral end of the tube, called pelvic opening or abdominal ostium, and measures about 2 mm in diameter.
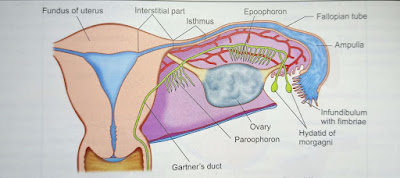 |
| Half of the uterine cavity and Fallopian tube of one side is cut open to show different parts of the tube. The vestigial structures in the broad ligament are shown |
Parts of the Fallopian tube
There are four parts, from medial to lateral they are:
- Intramural or interstitial lying in the uterine wall and measures 1.25 cm (1/2") in length and 1mm in diameter
- The isthmus is almost straight and measures about 2.5 cm (1") in length and 2.5mm in diameter
- Ampulla- tortuous part and measures about 5 cm (2") in length which ends in wide
- Infundibulum measuring about 1.25cm (1/2") long with a maximum diameter of 6 mm. The abdominal ostium is surrounded by a no. of radiating fimbriae, one of these is longer than the rest and is attached to the outer pole of the ovary called ovarian fimbria.
Structures- Fallopian tube consists of three layers
- Serous- consists of peritoneum on all sides except along the line of attachment of mesosalpinx.
- Muscular- arranged in two layers- outer longitudinal and inner circular.
- The mucous membrane is thrown into longitudinal folds. It is lined by columnar epithelium, partly ciliated, other secretory nonciliated, and 'peg cells'. The epithelium rests on dedicated vascular reticulum of connective tissue. There is no submucous layer nor any glands. Changed occurs in the tubal epithelium during the menstrual cycle but is less pronounced and there is no shedding.
Functions of the Fallopian tube
The functions of the tubes are:
- Transport of gametes
- to facilitate fertilization, and
- survival of the zygote through its secretion.
Blood supply and Nerve supply of Fallopian Tube
Arterial Blood supply is from the uterine and ovarian. Venous drainage is through the pampiniform plexus into the ovarian veins.
Nerve Blood Supply The nerve supply is derived from the uterine and ovarian nerves. The tube is very much sensitive to handling.

Post a Comment